By Susan Usher, Jean Huot, Jeffrey Barkun, Luc Valiquette
This case study, produced by Health Innovation Forum with contributions from Mr. Jean Huot, Chief Information Officer at the MUHC and CHUM, Dr. Jeffrey Barkun, Director, Division of General Surgery, MUHC, and Dr. Luc Valiquette, Director of the Department of Surgery at the Université de Montréal, examines the role of Chief Clinical Officer of Technological Transition created by Montreal’s academic health centres to guide IT implementation. — Produced as part of the MUHC-ISAI's 2010 program.
Challenge
Information technology (IT) projects have a notoriously high failure rate. The most frequent cause of failure is poor uptake by the front-end users. In health care, there is general consensus that clinicians need to be involved in all stages of IT implementation, but as yet few guidelines exist on how to do this.
In 2002, two of Montreal’s academic health centres, the McGill University Health Centre (MUHC) and the Centre hospitalier de l’Université de Montréal (CHUM), embarked on the process of defining and implementing clinical information systems that form the basis of an electronic patient record. The decision was part of major redevelopments at both centres that will see multiple hospital sites consolidated and new hospital construction. The MUHC and CHUM, each of which processes over 80 million electronic transactions a year, decided to work together on the modernization of information and communication technology.
Jean Huot had been Chief Information Officer (CIO) at the MUHC and Executive Director of SYSCOR, the MUHC’s Information Systems-Information Technology (IS-IT) partner, since 1998. In 2002, he also became CIO at the CHUM in order to lead the collaborative effort between the two health centres.
The broad aim is to acquire a state-of-the-art electronic health record with electronic prescribing and ordering, and create a clinical information system that will serve as an integration platform between internally collected data (the hospital-based electronic patient record, computerized physician order entry, requests) and data provided and used by external players (research, telehealth, the provincial health record and external healthcare providers). It is a complex, multi-year project that involves acquiring the basic clinical information system and implementing the electronic patient record; developing and integrating specialized modules into that system; digitalizing medical records (anticipating eventual connectivity between the record and biomedical equipment); and planning the technological infrastructure for the new hospitals.
The program
Mr. Huot and the Executive Directors of the MUHC and CHUM recognized the need to involve clinicians from the outset in what they broadly called the technological transition. “Clinician leaders are usually within the IT team,” says Mr. Huot. However, as the project picked up speed and gained clinical resonance, they felt that a stronger and more independent role was needed to ensure clinician empowerment and buy-in.
The position of Chief Clinical Officer of the Technological Transition was created in both institutions, with slight differences in mandate and reporting structure between the organizations. Coincidentally, two surgeons were appointed. Dr. Luc Valiquette is Director of the Department of Surgery at the Université de Montréal. Dr. Jeffrey Barkun is Director of the Division of General Surgery and Surgical Director of Quality at the MUHC. The two have provided clinical leadership on all aspects of the project, from the selection of the initial system through every stage of implementation.
“I am Chief Clinical Officer and clinical is the key word,” says Dr. Barkun. “I report directly to the MUHC’s Director General and CEO, not to IS-IT. And that was purposeful, so that a clinical vision of informatics — as a tool that has to make things safer for the patient, easier for the clinician, and contribute to teaching and research — is heard apart from IT concerns, which include but are not limited to where the computer is housed, how quick the wires are, what bandwidths are used, even how security is assured.”
The technological transition at the MUHC and CHUM is regarded first and foremost as a clinical project. It aims to improve the efficiency and coherence of work processes and clinical practices; facilitate the harmonization of practices; improve the communication of clinical information to care teams; reduce undesirable events and increase patient safety; and improve the quality of clinical documentation, notably by reducing the duplication of data entry. “It is there because it answers an objective that is meaningful to clinicians,” states Mr. Huot.
System selection
It took about four years after 2002 to get to Phase 0. “We started with an e-mail asking clinicians to identify which functionalities they would want [in a clinical information system],” recalls Dr. Barkun. “Then we made the rounds to speak to each department and assembled focus groups to help us confirm the selection. We invited information technology companies in to show their demos and collected feedback on those.” With that, the MUHC and CHUM were able to issue a Request for Proposals.
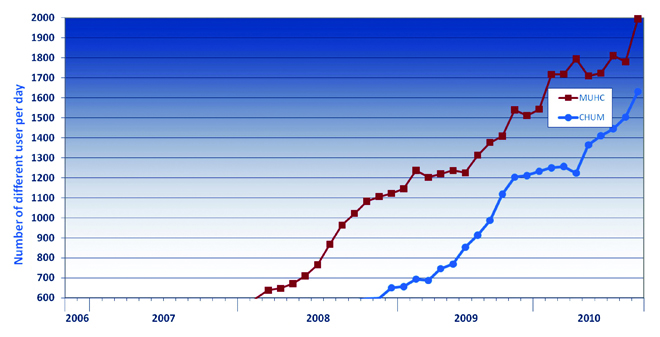
Dinmar’s Open Architecture Clinical Information System (OACIS) was chosen from among a number of bidders (Dinmar was bought by Emergis in 2006, which was then bought by TELUS in 2008), primarily for its ability to integrate various systems. The technological transition team has worked closely with the vendor to adjust OACIS to organizations’ needs as implementation proceeds. Figure 1 shows the uptake of the system at both the MUHC and the CHUM.
Productive relationships between clinical officers and IT are based on mutual respect for each other’s contribution. “They have a different culture and different preoccupations,” notes Dr. Barkun, “but my experience with the IT people and CIO has been fantastic. My job is to remind them to make sure the system helps clinical processes at all times.”
Staggered implementation
The implementation of OACIS at the MUHC and CHUM were 100% aligned. Working together, they could ensure they had a sufficient number of clinicians from each department to provide joint input into system design. A staggered implementation schedule was adopted so that one hospital would pilot a particular system and the other could learn from that experience. “We have a common executive clinical group,” says Dr. Valiquette, “that has been meeting together regularly for the last seven years as we develop the same project in parallel, with people from both hospitals working on each component regardless of which hospital is implementing it first.”
They started with the easiest part: the display of results in OACIS. These include the electronic master patient index, which electronically matches data from records belonging to an individual patient, regardless of the point of origin. “Patient demographics, a history of visits, laboratory, pathology, microbiology, medication profile, medical imaging, transcriptions and reports are now accessible in every hospital at both the CHUM and the MUHC by multiple physicians at the same time,” according to Dr. Valiquette. “And the integration of this information produced a very rapid benefit for clinicians.”
The team is now working on clinical documentation and computerized physician order entry programs. The MUHC now has 100% documentation of allergies for inpatients, according to Dr. Barkun, while the CHUM is taking on the scanning of paper charts to incorporate this information into the electronic record. The scanned reports will be displayed in a module of OACIS as a bridge measure that recognizes that information sources will not all be fully electronically linked for another few years. The MUHC is piloting medical imaging order entry and electronic documentation of vital signs and clinical measures, and will soon begin medication entry and discharge summary modules.
A team effort
“Each hospital has its own coordination body,” says Dr. Valiquette. “These are truly multidisciplinary: You cannot advance these projects if you do not work with everybody: administrators, IT people and all of the clinicians, not just physicians.” The coordination body helps stagger project implementation intelligently and pace it to recognize limitations in overall information system resources and in clinicians’ ability to incorporate changes. “Not only do you have to make sure that your project has a life of its own and speeds up clinical processes,” says Dr. Barkun, “you have to take into account the context of what is going on in the units where the modules are being implemented. If nurses have to learn how to use OACIS to document clinical metrics at the same time as new insulin pumps and new coagulation protocols are being instituted, they risk being overwhelmed.”
When introducing a new module, the OACIS team trains clinical champions, managers and ‘super-users’ so that they can then train personnel within each department. Training tools are also available through the MUHC and CHUM Intranet and all units are asked to review their workflow to include electronic documentation in OACIS. “The screen view and interface are set up by the clinical workgroups,” Dr. Barkun points out, “and have to be updated according to changes in practice.”
Dr. Valiquette and Dr. Barkun chair implementation committees, which meet monthly at both organizations. They are also responsible for identifying and cultivating other clinical champions at their respective hospitals and recruiting clinical representation from each department. This involves a constant process of generating discussion with clinicians to ensure their participation, and following up on concerns expressed about project evolution. This work is undertaken alongside their clinical, research, teaching and administrative responsibilities.
Communications
Mr. Huot stresses the need to empower these clinical working groups and clinical champions to help define the implementation strategy. “We need to make sure that the system addresses their priorities,” he says.
Two public relations and communications officers are dedicated to OACIS at both the MUHC and CHUM. “We work to promote OACIS both internally and externally,” says Chantal Beaudry, Public Relations and Communications Advisor, Technological Transition, CHUM-MUHC. “Our challenge is to develop communication plans that touch clinicians in their day-to-day activities and develop communication tools that facilitate organizational change.” This has helped prepare people for the different implementation phases, and provides a way to report on progress and recognize people who participate in pilots and other initiatives. Dr. Barkun and Dr. Valiquette hold Grand Rounds in all medical specialties on a regular basis to provide feedback and information to clinicians as the systems are implemented. “We use motivating communications, such as a news release when we reach certain landmarks in usage,” says Dr. Barkun. “And we have regular information sent out about OACIS in the MUHC internal newsletter to tell people what is coming next.” In 2008, the technological transition team organized a symposium that attracted some 400 participants, who were invited to visit the hospital sites and discuss the new technological tools with clinicians.
Uptake
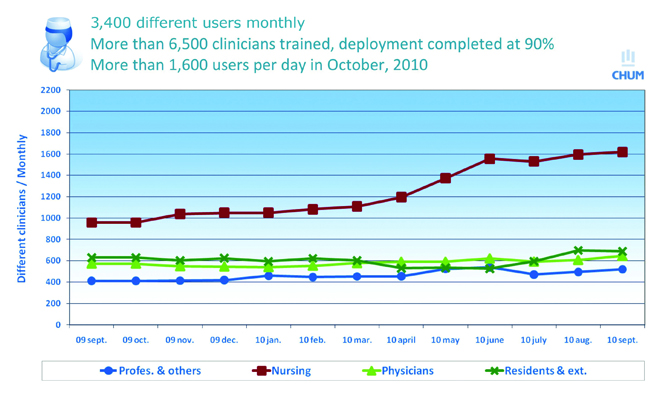
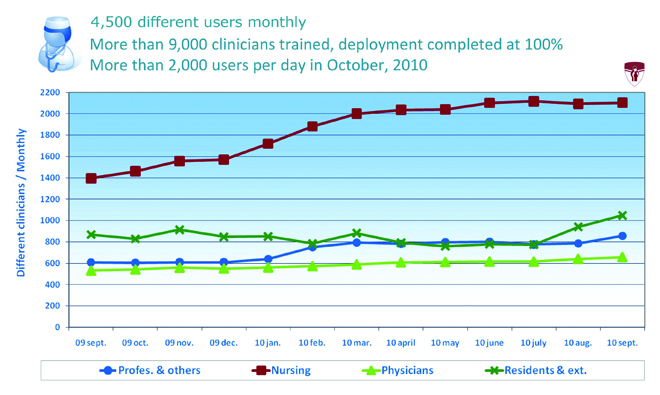
The Chief Clinical Officers are also responsible for monitoring use of the new systems and troubleshooting problems that arise. The number of users who sign on and the number of sessions that are opened each day are tracked. Users can be grouped by clinical category so uptake of each module can be tracked separately for nurses, interns and residents, clinicians and auxiliary services (Figure 2 and Figure 3). “If we see that user curves stop going up in a particular group,” says Dr. Barkun, “we go and find out why.”
By September 2010, over 9,000 clinicians at the MUHC had been trained and deployment of OACIS Phase 1 was complete. Between September 2009 and September 2010, the number of nurses using the system grew from 1,400 to 2,100, doctors from 500 to 650, resident and students from 900 to 1,050 and other professionals from under 600 to 850. At the CHUM, 6,500 clinicians had been trained in the use of OACIS as of September 2010, and deployment was 90% complete.
In May 2009, OACIS won the OCTAS award, the highest distinction for IT projects in Québec. Mr. Huot highlighted the technical features that distinguish OACIS, notably the ability to connect separate systems and preserve existing IT investments. However, the implementation process is an equally if not more important factor in the success. At the time of the award, Dr. Barkun recognized that it was made possible “by the participation of thousands of clinicians working in close partnership with technological and administrative members of the project.” According to Dr. Valiquette, “this award really shows that clinical users’ empowerment is instrumental to the success of such projects.”
Potential for expansion
Dr. Barkun and Dr. Valiquette have pioneered an important role in the implementation of clinical information systems and have a few overarching principles to share with others who may undertake similar roles.
1. The Chief Clinical Officer has to be the ‘straw man,’ i.e. to create easy mechanisms for people to express concerns and be accountable for addressing them.
2. It is important to recognize the strengths and weaknesses of the product and ensure that the vendor works to improve shortcomings.
3. Laggards should not be allowed to slow a project down.
4. The number of ‘clicks’ should always be minimized.
5. The fight should always be in the name of patient benefits.
Along with OACIS implementation, the Chief Clinical Officer at the MUHC is also responsible for prioritizing the development and implementation of specialized systems either as applications that reside within OACIS or as separate systems that interface with OACIS. Among the projects implemented to date at the MUHC are a specialized electronic health record in the ER and a system to manage all the information relevant to the operating rooms, from preoperative scheduling and operations to equipment management. Dr. Barkun acknowledges that prioritization is difficult: selecting these projects means that another project gets bumped for the time being. “The coordination group and I have to make decisions about what we think are more and less important priorities,” he says, “recognizing that there are only a certain number of IS-IT resources.” The MUHC’s budget for IT as a percentage of the overall budget is about half of what it is at other institutions in Canada.
Dr. Barkun will soon ask every clinical group at the MUHC what additional functions would make OACIS ‘fantastic’ for them. Responses will be prioritized and matched with hospital priorities, and members of these clinical groups will then be recruited to help develop clinical aspects of the system. “A few years ago,” he says, “clinicians did not really like information systems. OACIS has helped to change that. There are problems, but it is remarkable how few complaints I have had about the system. There was a major generational issue before, but as older clinicians retire and are replaced by younger ones who trained in hospitals with electronic health records, the challenge is no longer getting physicians excited, it is meeting their expectations.”
“The Chief Clinical Officer role opens the door to clinician interest in IT systems,” says Mr. Huot. “It will continue at least until the clinical information system is completely deployed, but I see it increasingly as a permanent role. Biomedical technology is evolving all the time and the Chief Clinical Officers are powerful allies in linking technological possibilities with clinical needs.”